Your Gums and Your Body: How Systemic Disease Rewrites the Rules of Gum Disease
Have you ever felt like you’re doing everything right for your oral health—brushing diligently, flossing daily—but your gums are still bleeding, receding, or just not getting better? It’s a frustrating experience, and it often feels like you’re missing a key piece of the puzzle.
Here’s a thought that might change how you see your health forever: the answer might not be in your mouth at all. It could be hidden in your broader health picture.
Your mouth is a window to your body's overall well-being. Far from being an isolated system, it’s deeply connected to your cardiovascular, endocrine, and immune systems. This article will explore how systemic conditions like diabetes, heart disease, and autoimmune disorders can fundamentally alter the progression, presentation, and even the diagnosis of gum disease, turning a seemingly straightforward oral health issue into a complex, whole-body challenge.
Foundation: The ""Common Soil"" of Inflammation
To understand this connection, we first need to grasp two core concepts and how they interact. Think of it as a garden: for a problem to grow, it needs the right soil.
First, let's clarify what is one potential consequence of poor oral hygiene: periodontal (gum) disease. It’s not just about plaque on your teeth. It’s a chronic inflammatory condition triggered by a bacterial imbalance. In its early stage, gingivitis, gums become red and swollen. Left unchecked, it can advance to periodontitis, where the inflammation destroys the tissues and bone that support your teeth, leading to tooth loss.
Second, we have systemic diseases—conditions that affect your entire body, such as diabetes, cardiovascular disease, or rheumatoid arthritis.
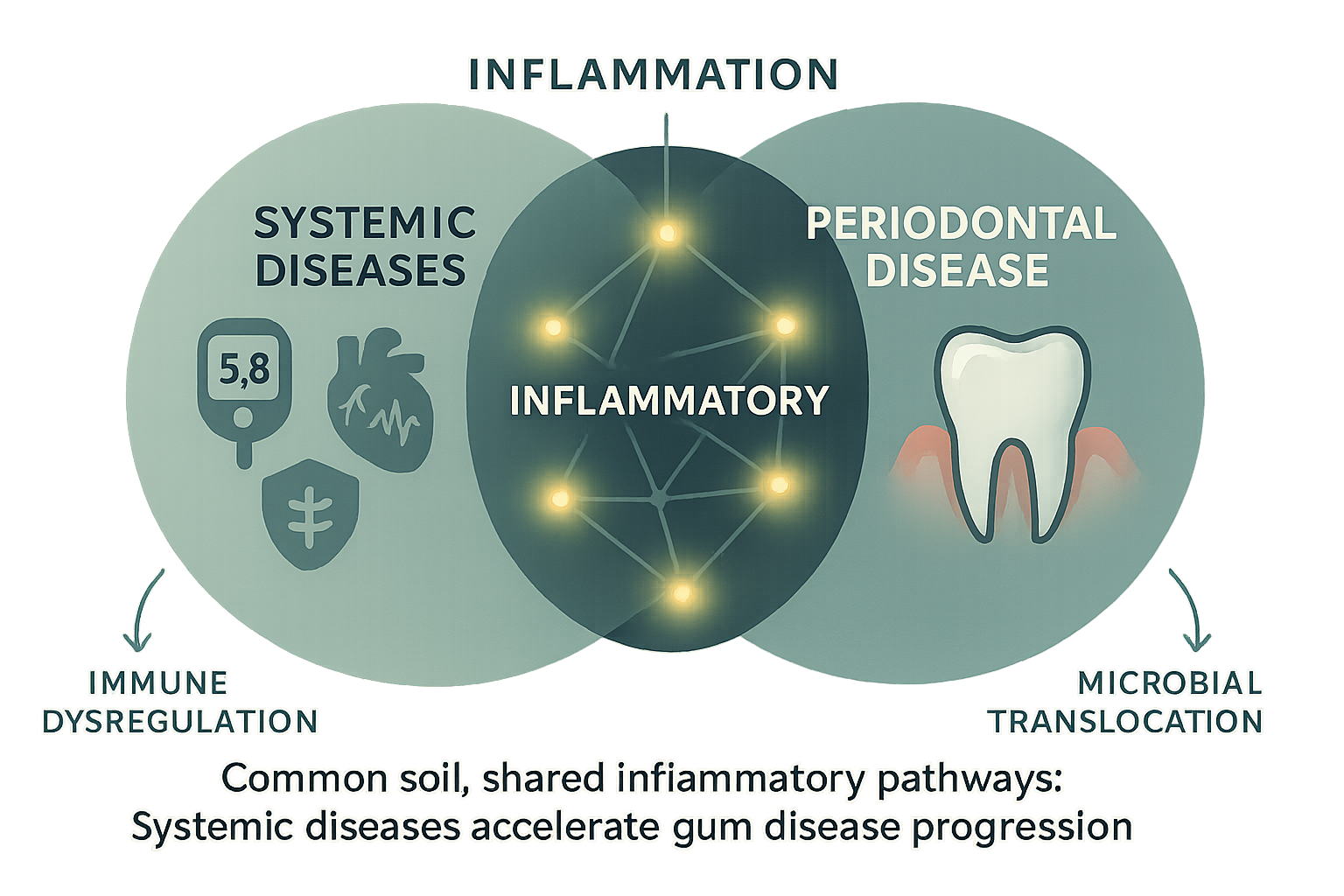
The crucial link between them is inflammation. It’s the ""common soil"" where both problems can take root and flourish. When your gums are chronically inflamed, inflammatory messengers (called cytokines) can escape into your bloodstream, contributing to inflammation throughout your body. Conversely, when your body is already dealing with systemic inflammation from another condition, your gums become far more vulnerable to bacterial attack. It’s a bidirectional relationship where each condition can fuel the other.
This infographic clarifies how systemic diseases like diabetes and cardiovascular conditions share inflammatory pathways with periodontal disease, creating a 'common soil' that accelerates gum disease progression.
When the Body's Signals Get Crossed: Key Systemic Modifiers
A systemic disease doesn’t just increase your risk for gum disease; it can change its very nature, acting as an accelerant, a disguise, or an amplifier. This is why a standard approach to gum disease often fails in systemically compromised individuals.
Uncontrolled Diabetes: The Accelerant
The link between diabetes and periodontitis is one of the most well-documented. Uncontrolled high blood sugar acts like a powerful accelerant for gum disease. Here’s why:
- It weakens your defences: High glucose levels impair the function of white blood cells, your body's primary defenders against bacterial infection.
- It fuels the enemy: The bacteria that cause gum disease thrive in a sugar-rich environment.
- It slows down repairs: Diabetes hinders the body's ability to heal and repair tissues, including your gums and the bone that supports your teeth.
Research from the American Academy of Periodontology shows that individuals with diabetes are up to three times more likely to develop periodontitis. For them, gum disease often progresses much faster and is more severe than traditional risk factors would suggest.
Cardiovascular Disease: A Two-Way Street of Inflammation
If you have cardiovascular disease, the systemic inflammation present in your body creates a state of high alert, making your gums more susceptible to infection. The connection also flows in the other direction. Bacteria from infected gums can enter the bloodstream (a process called bacteremia) and have been found in the fatty plaques that clog arteries in the heart, suggesting they may play a role in atherosclerosis.
Autoimmune Disorders (e.g., Rheumatoid Arthritis): A Confused Immune System
In autoimmune disorders like rheumatoid arthritis or lupus, the body's immune system mistakenly attacks its own healthy tissues. This same dysregulated immune response can target the gums and jawbone, leading to rapid and severe periodontal destruction that seems disproportionate to the amount of plaque present. The shared inflammatory pathways mean a flare-up in your joints could coincide with a worsening of your gum health.
The Hidden Impact of Medications
It’s not just the disease but also its treatment that can complicate the picture. Certain medications, like some blood pressure drugs (calcium channel blockers), anti-seizure medications, or immunosuppressants used after organ transplants, can cause gingival overgrowth. This makes gums swell and cover the teeth, creating deeper pockets where bacteria can hide and making effective cleaning nearly impossible.
The Diagnostic Dilemma: Why Standard Gum Disease Staging Can Fall Short
Traditionally, a dentist diagnoses and stages gum disease by taking physical measurements—using a small probe to measure the depth of the ""pockets"" between your teeth and gums and using X-rays to see how much bone has been lost. This creates a snapshot of the physical damage that has already occurred.
But what if that snapshot is misleading?
For a person with a compounding systemic condition, this standard approach can dramatically underestimate the disease's true severity and trajectory. The physical damage might look like Stage II, but the underlying ""silent fire"" of systemic inflammation could be driving the disease forward at the speed of a Stage IV case.
This diagnostic gap is critical. It can lead to:
- Under-staging: Classifying the disease as less severe than it is biologically.
- Ineffective Treatment: Prescribing a standard cleaning when a much more targeted and intensive therapy is required.
- Frustrating Outcomes: The patient follows the treatment plan perfectly, but the disease continues to progress because the root cause—the interplay with their systemic health—was never fully addressed.
This raises a crucial question: How can you accurately diagnose and treat gum disease when its very rules are being rewritten by a patient’s overall health?
Mastery: A More Precise Approach to Diagnosis and Treatment
The answer lies in moving beyond a one-size-fits-all approach and adopting a methodology that sees the full picture. It requires a deeper level of diagnostics and a more advanced set of therapeutic tools.
Seeing the Unseen: Beyond Standard Metrics
At The Behrens Dental Practice, the diagnostic process is built on the understanding that every patient's case is unique, especially when systemic factors are involved. Instead of relying solely on physical staging and grading, the first step is a Micro Perio Analysis. A key part of this is a microbiological DNA test to identify the exact types and quantities of harmful bacteria driving the infection.
Why is this so important? A patient with diabetes might be susceptible to a different, more aggressive cocktail of bacteria than a healthy individual. Knowing the specific pathogen allows for a truly personalized treatment plan that targets the precise cause of the disease, rather than just its symptoms.
Re-calibrating the Staging Process
With this detailed microbiological data, the clinical team can create a far more accurate diagnosis. They can see not just the existing damage but also the biological engine behind it. This allows them to grade the risk of future progression with much higher accuracy and create a treatment plan based on the unique interplay between the bacteria present and the patient's systemic health profile.
This flowchart educates on how practitioners modify traditional periodontal staging to incorporate systemic disease factors, employ Behrens' advanced diagnostics, and apply Duo-Lase treatment for precision care.
Precision Treatment for Complex Cases: The Duo-Lase™ Advantage
Once you have an accurate diagnosis, you need a treatment powerful enough to address the complexity of the case yet gentle enough to support a compromised healing system. This is where an innovative therapy like the Duo-Lase duo laser comes in. This non-surgical approach uses two distinct types of laser light to fight gum disease on two fronts:
1. Photo-Dynamic Pocket Decontamination: The first laser specifically targets and eliminates the harmful bacteria identified in the DNA analysis. Unlike traditional methods that can be less discriminating, this is a precise, targeted strike on the infection's source without the need for scalpels or sutures.
2. Bio-Stimulation: The second laser works at a cellular level to promote healing. It reduces inflammation and stimulates the production of collagen and new, healthy tissue. For a patient whose natural healing ability is impaired by a condition like diabetes, this bio-stimulation is a game-changer, helping the body repair itself more effectively.
This dual approach is uniquely suited for systemically compromised patients, offering a minimally invasive path to calming inflammation and regenerating tissue, which has led to a success rate exceeding 99% in saving teeth that might otherwise be lost.
Taking Control: Practical Steps for Your Oral and Overall Health
Understanding this connection is the first step toward better health. Here are actionable steps you can take.
Be a Thorough Historian
Always provide your dental team with a complete and updated medical history, including every diagnosis, medication, and supplement. Something you think is unrelated could be the key to understanding your oral health.
Connect the Dots
Pay attention to your body. Do you notice your gums bleed more during an autoimmune flare-up or when your blood sugar is high? Share these observations with your dentist and your doctor.
Ask the Right Questions
Advocate for your health by asking your dental provider:
- ""How might my medical condition be affecting my gum health?""
- ""Is my treatment plan specifically designed with my overall health in mind?""
- ""Are you able to identify the specific bacteria causing my infection?""
Explore Advanced Options
If you’re facing a complex case of gum disease, particularly with an underlying health condition, it’s worth learning more about comprehensive diagnostic approaches and modern therapies. You can find more information about treatments like the Duo-Lase treatment that are designed for these challenging situations.
Frequently Asked Questions (FAQ)
Q1: Can treating my gum disease actually help my other health conditions?
Yes. Because the relationship is bidirectional, reducing the body's inflammatory load by treating periodontitis can have a positive impact on other conditions. Studies have shown that effective periodontal therapy can help improve blood sugar control in people with diabetes and may reduce markers of inflammation related to cardiovascular disease.
Q2: My gums bleed, but I don't have any other health problems. Should I still be concerned?
Absolutely. Bleeding gums are never normal; they are a sign of active inflammation and infection. While it could be an isolated oral health issue, persistent gum disease can sometimes be one of the earliest signs of an undiagnosed systemic problem. It is crucial to address it before it progresses.
Q3: Is a treatment like the Duo-Lase™ duo laser painful?
The Duo-Lase™ duo laser is a minimally invasive procedure designed to maximize comfort. Most patients report little to no pain during or after the treatment and experience a much faster and more comfortable recovery compared to traditional gum surgery.
Q4: How do I know if my dentist is considering my systemic health?
A proactive dental team will take a comprehensive medical history and ask detailed follow-up questions about your conditions and medications. A key indicator of a truly holistic approach is the use of advanced diagnostics, like microbiological analysis, to understand the root cause of your disease and tailor a treatment plan that accounts for your entire health profile.
Your Health is a Single, Interconnected Story
Your body is not a collection of separate parts. It is one integrated system where the health of one area profoundly impacts the health of another. Your gums are on the front line of this interaction, often reflecting the first signs of a deeper imbalance.
Ignoring this connection can lead to years of frustrating and ineffective treatment. However, embracing it—by seeking a diagnosis that sees the whole picture and a treatment designed to address its full complexity—is the first and most critical step toward achieving true oral and overall wellness."