Your Dental Implant Is In, But Is It Safe? A Guide to Peri-Implantitis.
You’ve made a significant investment in your smile with a dental implant. It feels strong, looks natural, and is widely considered the gold standard for replacing a missing tooth. The common assumption is that once it's in, it's a permanent, maintenance-free solution. But what if the very foundation holding that marvel of modern dentistry in place—the gum and bone—is silently coming under attack?
This is the reality of peri-implant disease, an inflammatory condition that behaves like gum disease but targets dental implants. It’s a topic that often surprises patients, who believe their artificial tooth is immune to the problems that affect natural teeth. The truth is, while an implant can't get a cavity, the living tissue around it is very much vulnerable.
Understanding the signs, stages, and unique nature of this condition is the single most important thing you can do to protect your investment and your oral health for a lifetime.
A Tale of Two Foundations: Mucositis vs. Peri-Implantitis
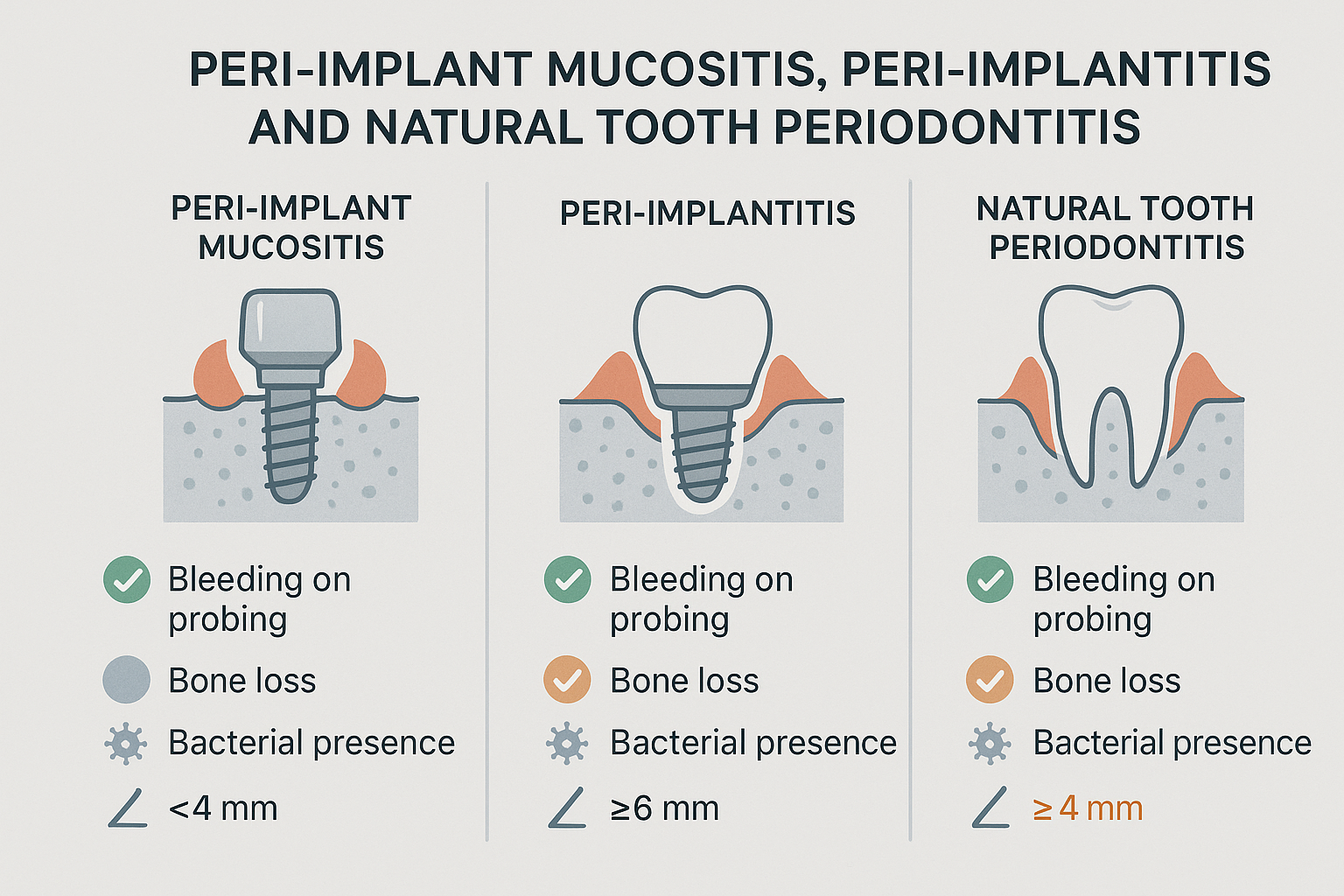
Just like with natural teeth, problems around implants begin with inflammation caused by a buildup of bacterial plaque. However, these issues fall into two distinct categories: peri-implant mucositis and its more destructive successor, peri-implantitis.
Peri-Implant Mucositis: Think of this as the equivalent of gingivitis for an implant. It’s a reversible inflammatory reaction in the soft tissues surrounding the implant. You might notice some redness, swelling, or slight bleeding when you brush. At this stage, there is no bone loss, and the implant's stability is not yet compromised. With professional cleaning and improved oral hygiene, mucositis can often be fully resolved.
Peri-Implantitis: This is the real threat. If mucositis is left untreated, it can progress to peri-implantitis, a condition where the inflammation spreads deeper, leading to the deterioration of the bone supporting the implant. This bone loss is irreversible and, if it continues, will cause the implant to become loose and ultimately fail.
The challenge is that peri-implantitis often develops silently, with little to no pain in its early stages. This is why understanding the risk and attending regular dental check-ups is paramount.
The Silent Progression: Why This Condition Is So Deceptive
Peri-implant diseases are surprisingly common. Research from the Journal of Dental Research suggests that while peri-implantitis affects a significant number of patients (around 22%), its precursor, peri-implant mucositis, is far more widespread, impacting nearly half of all individuals with implants.
This creates a crucial window of opportunity. By catching and treating mucositis early, we can prevent the devastating bone loss of peri-implantitis from ever occurring. Ignoring those first subtle signs of bleeding or puffiness around an implant allows harmful bacteria to thrive. Indeed, understanding what is one potential consequence of poor oral hygiene is just as critical for an implant as it is for a natural tooth, as it can lead to a cascade of inflammation that puts your entire investment at risk.
The anatomy around an implant is different from that of a natural tooth. The seal of the gum tissue is less robust, and the blood supply is less rich, making it more susceptible to bacterial invasion and slower to heal. This means that once bone loss starts, it can progress much more rapidly and aggressively than traditional periodontitis.
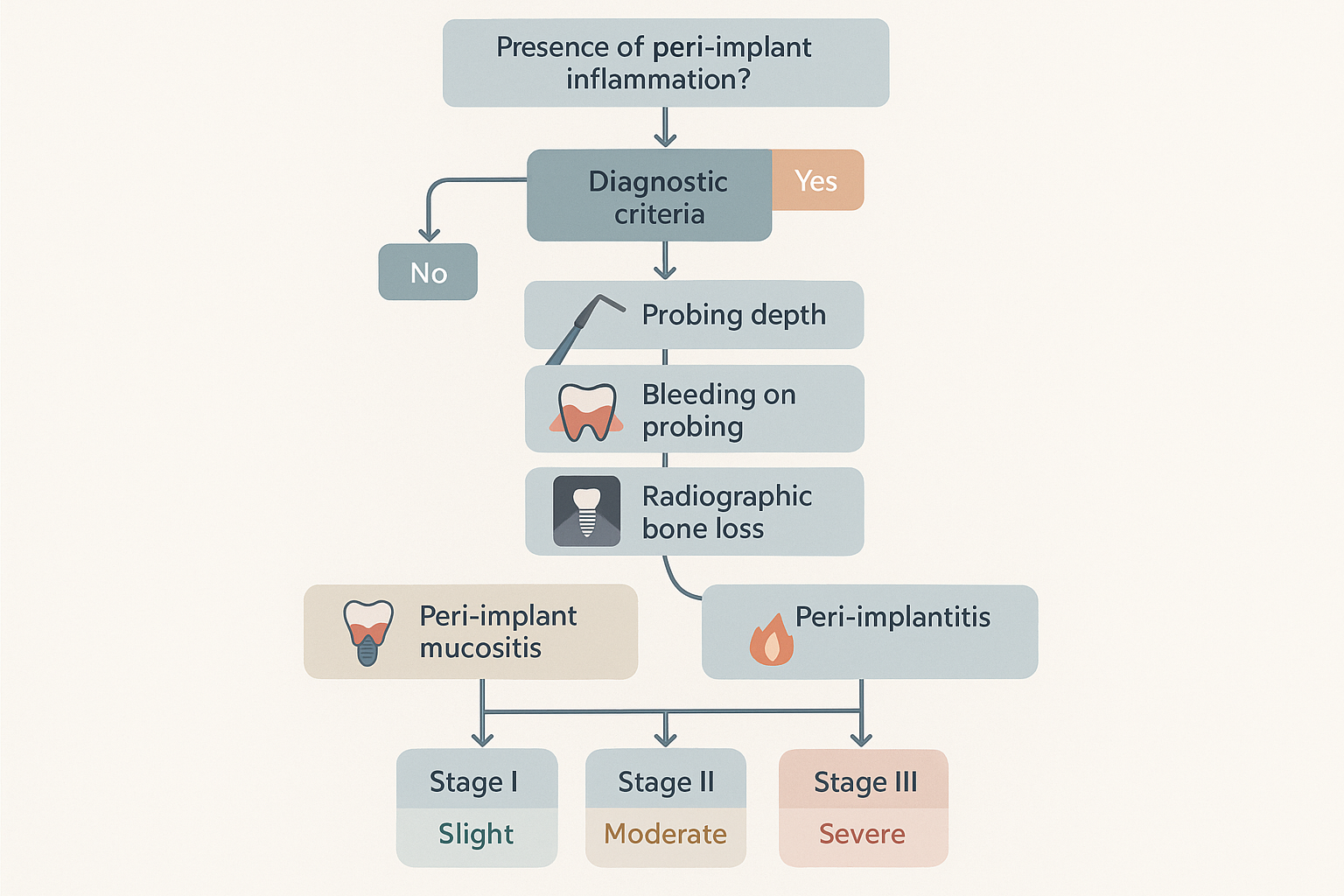
A Clinician's Roadmap: How We Diagnose and Stage Peri-Implantitis
Identifying peri-implant disease isn't a simple glance-and-guess process. It requires a systematic, multi-faceted approach to accurately assess the health of the surrounding tissues and bone. At The Behrens Dental Practice, we take this a step further by not only staging the disease but also performing microbiological tests to pinpoint the exact bacteria causing the infection, allowing for a truly customized treatment plan.
Here’s a look at the key steps involved in a thorough diagnosis.
Probing the Depths (PD)
A clinician will use a special, gentle instrument called a periodontal probe to measure the depth of the "pocket" or sulcus between the implant and the surrounding gum tissue. Healthy pockets are typically shallow. An increase in probing depth over time is a red flag, indicating that the supporting tissues may be detaching from the implant surface. Establishing a baseline measurement shortly after the implant is restored is critical for tracking changes over time.
Bleeding on Probing (BoP)
This is one of the earliest and most reliable indicators of inflammation. During the probing process, the clinician will watch for any signs of bleeding. While its presence confirms inflammation (mucositis or peri-implantitis), its absence is a strong sign of healthy tissue. If your gums bleed around your implant when you brush or during a dental exam, it’s a clear signal to take action.
Assessing Bone Loss with Radiographs (X-rays)
Because the most significant damage happens beneath the gum line, radiographs are essential for a definitive diagnosis of peri-implantitis. X-rays allow the clinician to visualize the bone level around the implant and compare it to previous images. Any noticeable loss of bone height confirms that the disease has progressed from mucositis to peri-implantitis.
Based on these findings—probing depth, bleeding, and the extent of radiographic bone loss—a clinician can stage the severity of the peri-implantitis, typically classifying it as early, moderate, or advanced. This staging determines the most appropriate course of treatment to halt the disease and save the implant.
Not All Gums Are Created Equal: Implants vs. Natural Teeth
It’s easy to think of peri-implantitis as just "gum disease around an implant," but there are critical differences that both patients and clinicians must appreciate. The unique biology of the implant-tissue interface presents distinct challenges.
Tissue Structure: A natural tooth is connected to the bone by a network of fibers called the periodontal ligament, which provides a flexible, shock-absorbing cushion and a rich blood supply. An implant, on the other hand, fuses directly to the bone (a process called osseointegration) and lacks this ligament. The gum tissue fibers run parallel to the implant rather than inserting into it, creating a weaker biological seal against bacteria.
Disease Progression: Due to the less robust tissue seal and different blood supply, peri-implantitis can advance much more rapidly and with a more destructive pattern than periodontitis around natural teeth. The bone loss often appears as a crater-like defect, which can be difficult to treat.
Treatment Approach: While the goal—eliminating bacteria and stopping inflammation—is the same, the methods differ. Cleaning a contaminated implant surface without damaging it requires specialized instruments and techniques. Advanced non-invasive methods, such as the dual-laser technology used in a duo lase treatment, are designed to decontaminate these sensitive surfaces and stimulate healing in the surrounding tissues effectively.
Frequently Asked Questions (FAQ)
What are the main symptoms of peri-implantitis I should look for?
Early stages are often silent, but be aware of red, swollen, or tender gums around the implant; bleeding when brushing or flossing; a bad taste coming from the implant area; or a feeling that the implant or crown is becoming loose.
Can peri-implantitis be cured?
The bone loss from peri-implantitis is generally irreversible. However, the disease can be arrested. The goal of treatment is to stop the progression of bone loss, eliminate the inflammation, and maintain the implant for as long as possible. Early intervention gives the best prognosis.
How can I prevent peri-implant disease?
Prevention is a partnership between you and your dental team. It requires:
Meticulous Home Care: Brushing twice a day and cleaning between the implant and adjacent teeth daily with tools like water flossers, interdental brushes, or implant-specific floss.
Regular Professional Maintenance: Attending regular check-ups and hygiene appointments is non-negotiable. A professional can clean areas you can't reach and spot the earliest signs of trouble.
Managing Risk Factors: Conditions like smoking, uncontrolled diabetes, and a history of severe periodontitis increase your risk.
Is peri-implantitis painful?
One of the biggest dangers of peri-implantitis is that it is often painless until it reaches an advanced stage. This is why you cannot rely on pain as an indicator of a problem. Consistent monitoring by a dental professional is the only way to ensure it's caught early.
Your Next Step to a Healthy, Long-Lasting Implant
Your dental implant represents a fusion of biology and technology, but its success ultimately depends on the health of its living foundation. Peri-implant disease is a serious threat, but it is not inevitable.
By understanding the difference between mucositis and peri-implantitis, recognizing the importance of early detection, and committing to a diligent care routine, you can take control of your implant’s future.
If you have any concerns about your dental implant—whether it's slight bleeding, a change in appearance, or simply the desire for a comprehensive health check—the most powerful step you can take is to seek a professional evaluation. A thorough assessment is the best way to ensure your smile remains as strong and healthy as the day it was restored.