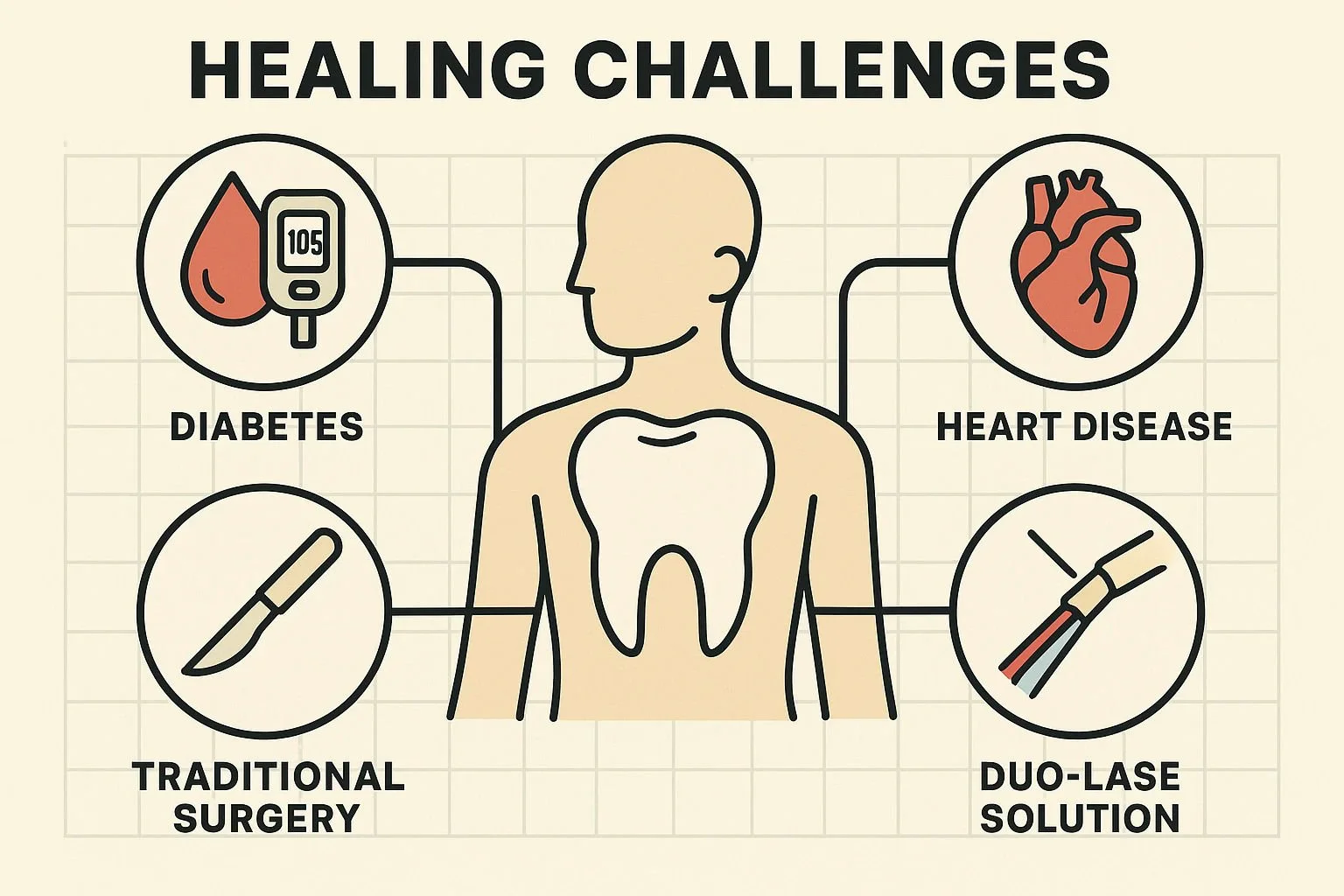
Gum Treatment Safety for Diabetes and Heart Disease
Is Gum Treatment Safe for Me? Navigating Recovery with Diabetes or Heart Conditions
For many people, a diagnosis of gum disease comes with a heavy dose of anxiety. But for those managing chronic health conditions like diabetes or heart disease, that anxiety is often compounded by a very specific fear: "Is the treatment safer than the disease?"
If you have been told you need gum surgery but are worried about how your body will handle the stress, bleeding, or healing process, you are not alone. It is a valid concern. Traditional dental surgery often requires stopping blood thinners or managing the risk of infection—complications that high-risk patients understandably want to avoid.
However, the landscape of dental care has shifted dramatically. We have moved from an era of "cutting and stitching" to an era of light and energy.
The Hidden Connection: Why Oral Health is Systemic Health
Before diving into treatment options, it is crucial to understand why treating gum disease is non-negotiable, especially for those with underlying conditions. The mouth is not an isolated ecosystem; it is the gateway to the rest of your body.
For patients with diabetes, the relationship is bidirectional. Uncontrolled gum disease creates inflammation that can cause blood sugar levels to spike, making diabetes harder to manage. Conversely, high blood sugar impairs the body's ability to heal gums.
For patients with heart disease, the bacteria responsible for gum infections can enter the bloodstream (a condition called bacteremia), potentially contributing to arterial plaque buildup or inflammation of heart vessels.
Ignoring the gums to avoid surgery isn't a safe option—it actually increases your systemic risk. The goal, then, is to find a treatment method that effectively eliminates bacteria without putting your body under unnecessary stress.
The Traditional Challenge vs. The Laser Solution
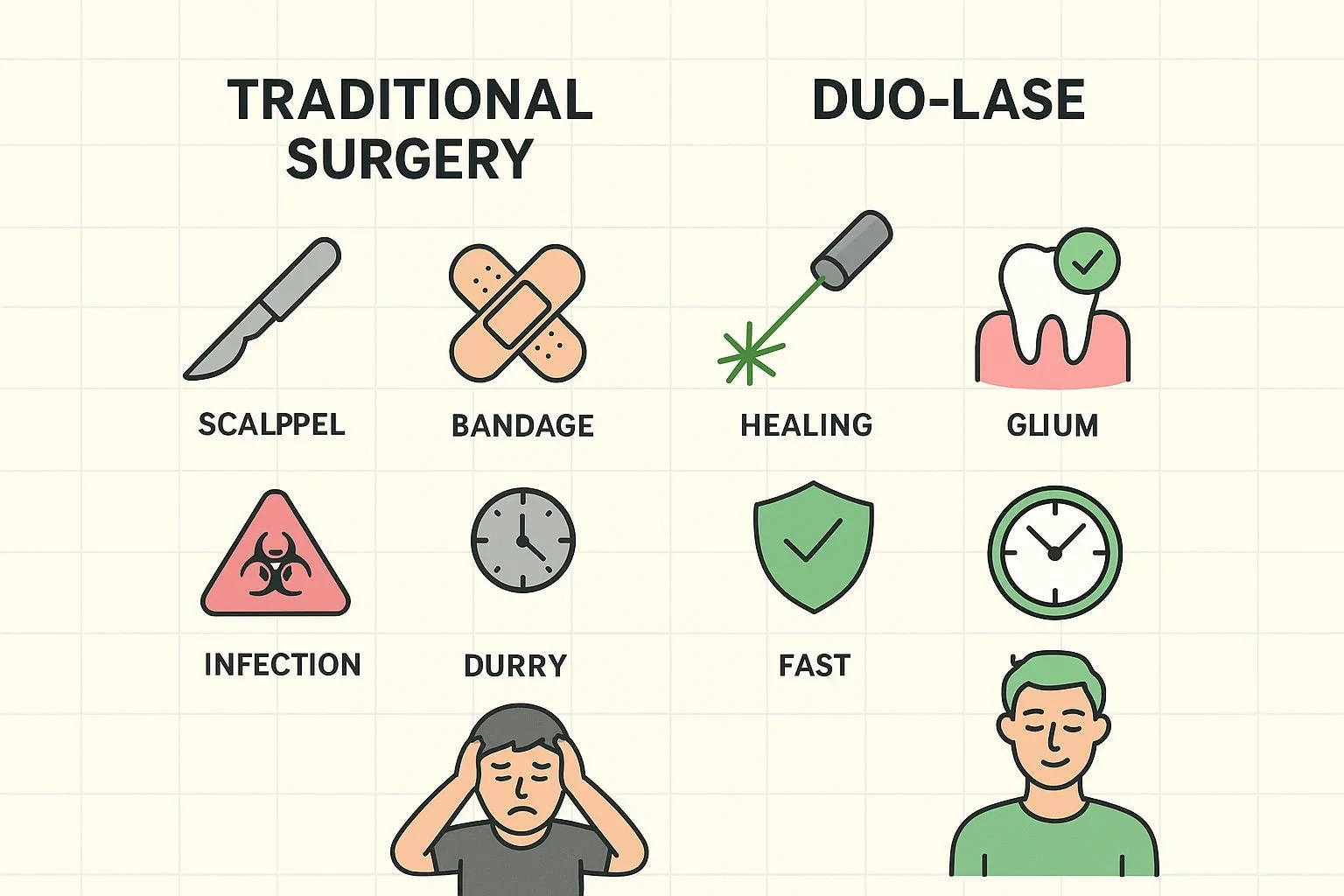
Historically, treating moderate to advanced periodontitis involved scalpel surgery. The dentist would cut the gum tissue to pull it back, clean the roots, and stitch it back together.
For a healthy patient, this is uncomfortable. For a medically compromised patient, it presents three hurdles:
Bleeding: A major concern for those on anticoagulants (blood thinners).
Infection: Open wounds are entry points for bacteria, a risk for those with weakened immune systems.
Slow Healing: Diabetes restricts blood flow, turning a standard recovery into a weeks-long ordeal.
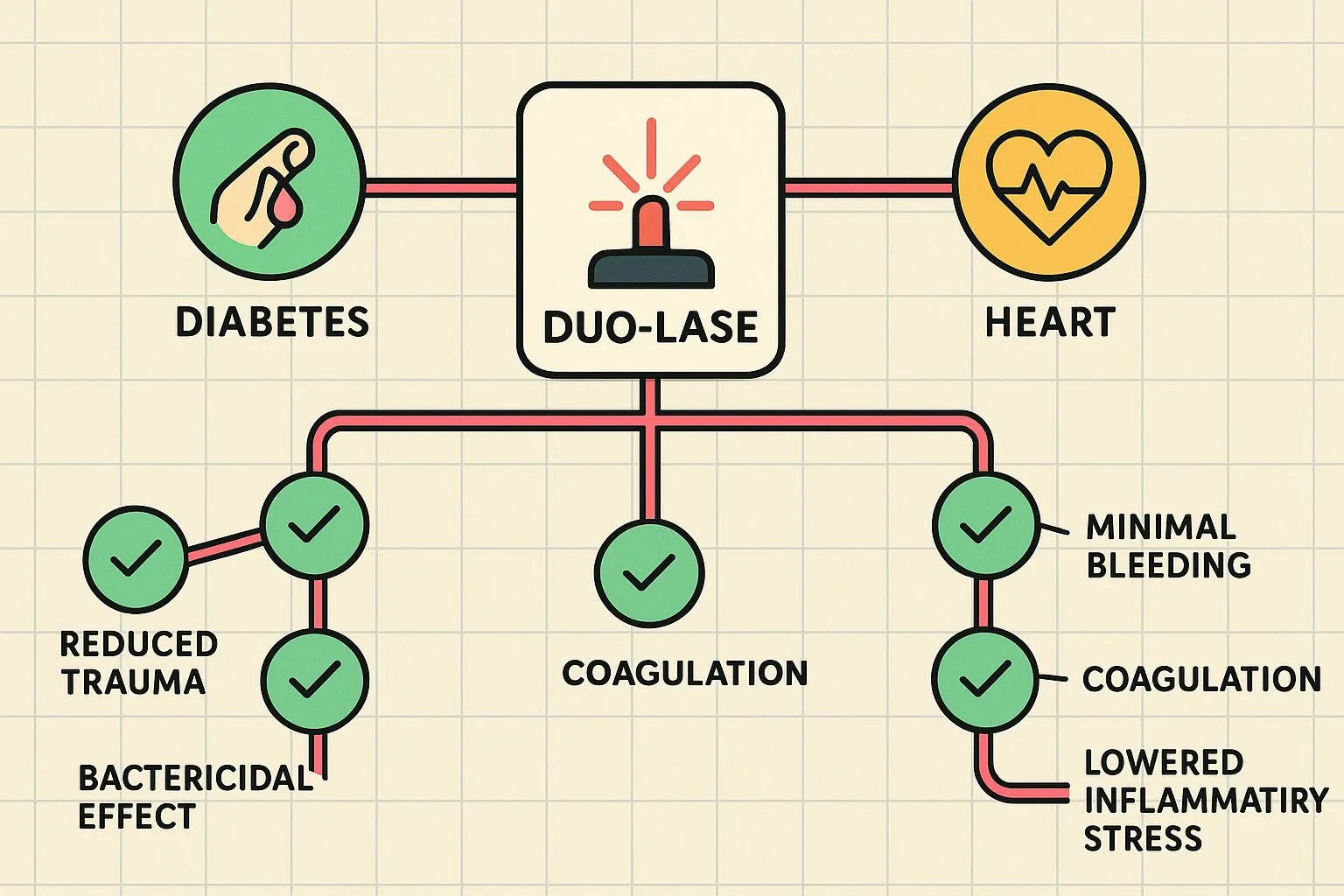
Enter Duo-Lase™: A Dual Approach to Healing
This is where technologies like duo-lase change the narrative. Unlike traditional tools that rely on mechanical scraping and cutting, Duo-Lase™ utilizes distinct laser wavelengths to address the disease without the trauma.
Specific Considerations for Your Condition
When considering laser periodontal treatment London based experts emphasize that the mechanism of healing is just as important as the bacterial removal. Here is how this technology specifically interacts with common health conditions.
For Patients with Diabetes
The Challenge: High glucose levels can make blood vessel walls stiffer and slow down the delivery of nutrients to a wound site. This "lazy" healing response is why diabetics are often prone to post-surgical infections.
The Laser Advantage: Duo-Lase™ employs a concept called "Bio-Stimulation." One of the laser wavelengths used doesn't just clean; it penetrates the tissue to stimulate the mitochondria (the power plant) of your cells. This helps "wake up" the healing process, encouraging collagen production and tissue regeneration even in bodies that typically heal slowly. By avoiding open incisions, the risk of opportunistic infection drops significantly.
For Patients with Heart Disease
The Challenge: Many heart patients take anticoagulants (like Warfarin or aspirin) to prevent clots. Traditional dentists often require patients to stop these medications before surgery to prevent excessive bleeding—a scary proposition that increases stroke risk.
The Laser Advantage: In many cases, laser gum treatment London practitioners find that patients do not need to alter their heart medication regimens (though consultation with your cardiologist is always required). Furthermore, the procedure is faster and less traumatic, reducing the physical stress on the heart during the appointment.
What Recovery Actually Looks Like
If you have researched stage 3 periodontal disease, you might be expecting a recovery involving painkillers, swelling, and a liquid diet.
With laser-assisted therapy, the recovery curve is flattened.
0-24 Hours: You may experience mild sensitivity, but because there are no sutures pulling on your gums, acute pain is rare. Most patients return to work the next day.
Day 3-7: While the gums are healing from the inside out, the surface remains intact. The "Bio-Stimulation" continues to work at a cellular level, accelerating tissue reattachment.
Long Term: Because the bacteria load is significantly reduced without destroying healthy tissue, the likelihood of gum recession (long teeth) is minimized compared to traditional surgery.
Please note that several laser sessions are necessary depending on each patient case.
Empowering Yourself: A Patient Checklist
If you are managing a systemic condition, your dental care requires coordination. When researching the duo lase cost or value, remember that safety is the ultimate metric.
Bring these questions to your next consultation:
Ask the Dentist: "Do you use Microbiological DNA analysis? I need to know exactly which bacteria are causing my infection so we can target them efficiently."
Ask your Physician/Cardiologist: "I am considering a laser-based dental procedure that involves minimal bleeding. Do I still need to adjust my anticoagulant medication?"
Ask your Endocrinologist: "My dentist plans to treat my periodontal inflammation. Should we monitor my HbA1c levels more closely in the months following treatment?"
Frequently Asked Questions
Is laser dentistry safe for pacemakers?
Generally, yes. Dental lasers are different from electrosurgery devices and typically do not interfere with pacemakers. However, you must always inform your dental team about your device so they can take appropriate precautions.
Will the laser hurt if I have sensitive gums due to diabetes?
Duo-Lase™ is often described as much more comfortable than traditional deep cleaning. The laser energy is highly targeted, meaning it removes diseased tissue while leaving healthy, sensitive tissue alone. Anesthetic is used to ensure you are completely comfortable throughout.
Can treating my gums actually lower my blood sugar?
Research suggests that treating gum disease can improve glycemic control. By reducing the chronic inflammation in your mouth, you reduce the body's overall inflammatory burden, which can help insulin work more effectively.
How do I know if the treatment worked?
The Behrens Dental Practice utilizes a rigorous protocol involving follow-up microbiological tests. They don't just guess; they test to ensure the specific bacteria causing your disease have been eliminated, providing peace of mind for high-risk patients.
---
Taking the Next Step
Your health history shouldn't disqualify you from saving your teeth. In fact, your overall health depends on it. By choosing a method that respects your body's physiology—minimizing trauma and maximizing healing—you can address advanced periodontitis without the fear of traditional surgery.
If you are ready to learn how laser therapy can fit into your wider health management plan, we invite you to explore the science behind Duo-Lase™ further.