Why Gum Disease Often Goes Unnoticed Without Pain
Silent Progression: Why Gum Disease Often Goes Unnoticed Without Pain
For most of our lives, we are taught that pain is the body’s ultimate alarm system. If you touch a hot stove, your hand recoils instantly. If you sprain an ankle, the sharp throb tells you to stop walking. We rely on this signal to tell us when something is wrong. However, when it comes to your oral health, relying on pain as a warning sign is a dangerous strategy. Periodontal disease is often referred to as a "silent thief" because it can steal your bone, gum tissue, and eventually your teeth without ever causing a physical ache until the damage is severe.
The absence of pain does not equal the presence of health. This disconnect is one of the most significant barriers to early treatment. Many patients sit in the dental chair, shocked to learn they have advanced bone loss, simply because nothing hurt. Understanding the reality of this condition and dispelling common myths about gum disease is the first step toward protecting your smile. If you are waiting for your gums to hurt before seeing a professional, you may be waiting too long.
The Science of Silence: Why It Doesn’t Hurt
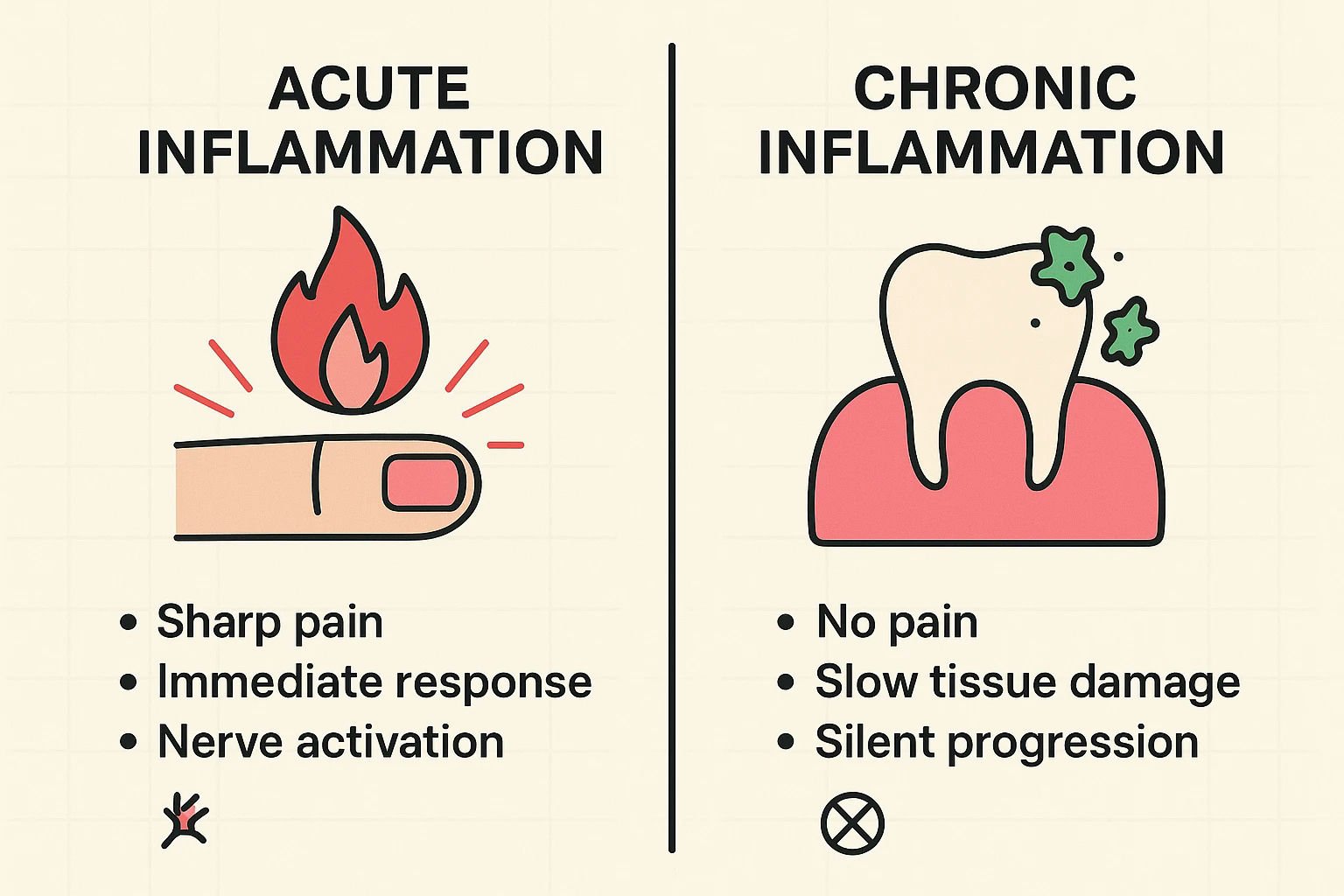
To understand why your gums can deteriorate without pain, we have to look at the biology of inflammation. When you cut your finger, you experience "acute inflammation." The body rushes blood to the area, swelling occurs rapidly, and nerve endings (nociceptors) are triggered immediately to tell you to protect the injury. It is loud, fast, and painful.
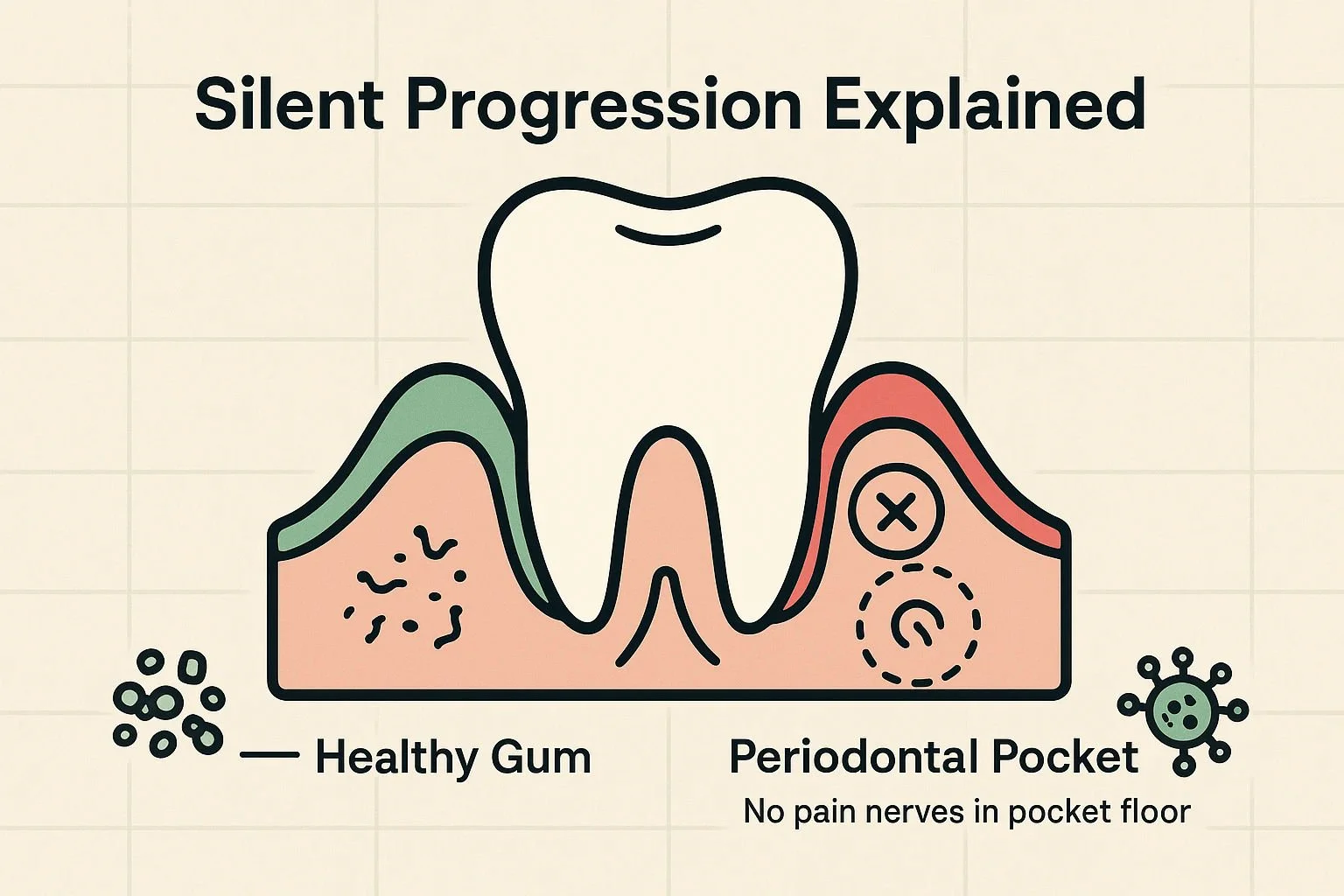
Gum disease, however, is a "chronic inflammatory" condition. It happens slowly, often over years. Research indicates that the specific environment inside gum pockets creates a unique biological situation. The bacteria that cause periodontal disease—specifically anaerobic bacteria that thrive without oxygen—trigger an immune response that breaks down tissue gradually.
During this chronic process, the body attempts to "wall off" the infection rather than fighting it with the explosive force used for a cut finger. This creates a state of localized hypoalgesia, where the pain-causing factors are counteracted by inhibitory mechanisms. Essentially, your body is managing the infection in a way that bypasses the pain alarms. This allows the disease to destroy the ligaments and bone holding your teeth in place while you feel perfectly fine.
The Real Warning Signs (Since Pain Isn't One)
If you cannot rely on pain, what should you look for? The symptoms of gum disease are often visual or social, rather than physical sensations. Recognizing these signs early can mean the difference between a simple cleaning and complex therapy.
1. "Pink in the Sink"
The most common early sign is bleeding while brushing or flossing. Many people ignore this or assume they just brushed too hard. In reality, healthy gums do not bleed. Bleeding is the body's way of signaling that the tissue is ulcerated and infected. If your hands bled every time you washed them, you would rush to a doctor; your gums should be treated with the same urgency.
2. Persistent Bad Breath
We aren't talking about "morning breath" or the aftereffects of a garlic lunch. Gum disease bad breath (halitosis) is caused by the volatile sulfur compounds released by the bacteria residing deep under the gum line. If mouthwash and brushing don't resolve the odor, it is likely originating from an infection that a toothbrush cannot reach.
3. Gum Recession and "Long" Teeth
As the bone supporting the teeth is destroyed, the gum tissue often follows, pulling back and exposing the root of the tooth. This can make teeth appear longer than they used to. While this can sometimes cause sensitivity to cold, it is often painless, further masking the severity of the issue.
4. Changes in Bite or Tooth Position
In later stages, such as stage 3 periodontal disease or advanced periodontitis, you might notice that your teeth feel loose or that your bite feels "off" when you close your mouth. This indicates that the bone support has been compromised significantly.
The Risk of Waiting
The statistics are sobering: over 42% of adults over the age of 30 have some form of periodontal disease. Because the progression is silent, many people unknowingly move from gingivitis (reversible) to moderate periodontitis (irreversible bone loss) without seeking help.
It is also important to consider the people around you. Many patients ask, "can you catch gum disease?" While not contagious in the same way as a flu virus, the bacteria that cause periodontal disease can be transferred through saliva. Ignoring your own silent symptoms can affect your partner’s oral microbiome as well.
Moving Beyond the "Wait and See" Approach
You cannot diagnose gum disease in the mirror, and you certainly cannot diagnose it by how you feel. The only way to know the true health of your gums is through professional evaluation.
At The Behrens Dental Practice, we believe in looking deeper than the surface. Our approach to gum health moves beyond basic cleaning to address the root cause of the disease:
Microbiological Analysis: We don't just guess; we test. By identifying the specific bacteria causing your infection, we can tailor a treatment plan effectively.
Staging and Grading: We accurately assess the level of damage to create a roadmap for recovery.
Duo-Lase™ Therapy: Our periodontal experts utilize advanced dual-laser technology to eliminate bacteria and stimulate healing. This approach is minimally invasive, avoiding the cutting and sutures associated with traditional gum surgery, making the treatment process as comfortable as possible.
Frequently Asked Questions
Why do my gums bleed but not hurt?
Bleeding is a sign of active inflammation and ulceration in the gum pocket. The lack of pain is due to the chronic nature of the disease, which suppresses the body's acute pain response mechanisms. Bleeding is your primary warning sign.
Can gum disease be cured?
Gingivitis (the early stage) is reversible. Periodontitis (where bone is lost) cannot be strictly "cured" in the sense that lost bone grows back on its own, but it can be halted and managed. With treatments like Duo-Lase™, we can eliminate the infection and stabilize the condition, preventing tooth loss.
Is gum disease hereditary?
Genetics play a role in how your body reacts to bacteria, but the disease itself is caused by plaque and tartar buildup. Even if you are genetically predisposed, proper hygiene and professional care can prevent the disease from progressing.
What happens if I ignore the symptoms?
Untreated gum disease leads to progressive bone loss, tooth mobility, and eventually tooth loss. It has also been linked to systemic health issues, including heart disease and diabetes.
Taking the Next Step
If you have noticed what gum disease looks like—bleeding, recession, or persistent bad breath—do not wait for pain to validate your concern. The silence of the disease is its most effective weapon. By scheduling a consultation with the periodontal experts at Behrens Dental Practice, you can get a clear picture of your oral health and access advanced, comfortable solutions to preserve your smile for life.