Beyond Bleeding Gums: Understanding Stage 2 Periodontitis
Have you ever noticed a little pink in the sink after brushing your teeth and thought, "It's just a bit of bleeding, no big deal"? It’s a common moment many of us dismiss. But what if that small sign is your body’s quiet alarm bell, signalling a critical shift happening just below the gumline?
This is the subtle, often silent transition from reversible gingivitis to Stage 2 periodontitis—the first stage where the damage becomes permanent. This isn't just about sensitive gums anymore. It's the point where the infection begins to break down the very structures that hold your teeth in place. Understanding this stage is the key to stopping gum disease in its tracks and saving your smile for a lifetime.
From Reversible Redness to Lasting Damage: The Tipping Point
Gingivitis, the earliest form of gum disease, is essentially a cry for help from your gums. It's characterised by redness, swelling, and bleeding, caused by a buildup of plaque bacteria. At this stage, the issue is confined to the gum tissue, and the damage is completely reversible with improved oral hygiene and professional cleaning.
But when left unaddressed, the balance of bacteria in your mouth shifts. More aggressive, destructive bacteria begin to thrive, triggering a chronic inflammatory response from your immune system. This is the tipping point where gingivitis progresses into Stage 2, or early, periodontitis.
The defining event of this stage is connective tissue destruction. Your body, in its effort to fight the persistent bacterial infection, begins to inadvertently destroy the ligaments and bone that anchor your teeth. This process is silent but measurable.
Here’s what that looks like clinically:
Clinical Attachment Loss (CAL) of 1–2 mm: Imagine the gum around your tooth is like a snug turtleneck jumper. CAL means that jumper has started to stretch and detach from the neck (your tooth) by 1-2 millimetres. This loss is irreversible.
Probing Depths of 4–5 mm: A dentist measures the tiny space between your tooth and gum, called a sulcus. A healthy sulcus is 1-3 mm deep. In Stage 2, this space deepens into a "periodontal pocket" of 4-5 mm, creating a haven where harmful bacteria can multiply, safe from your toothbrush.
Early Bone Loss: For the first time, the bone supporting your teeth begins to erode. On an X-ray, this shows up as bone loss in the upper third (coronal third) of the tooth root, but it’s less than 15%.
This isn't just a deeper cleaning issue anymore; it's a structural problem that, if ignored, will only worsen.
Symptoms of Early Periodontitis You Shouldn’t Ignore
While Stage 2 can be sneaky, your body does send out warning signals. Recognizing them is your best defence.
Persistent Bleeding Gums: If your gums bleed every time you brush or floss, it's not a sign of brushing too hard—it's a sign of active inflammation.
Red, Puffy, or Tender Gums: Healthy gums are firm, pink, and don't hurt. Inflamed gums are a hallmark of periodontal infection.
Bad Breath That Won't Go Away (Halitosis): The bacteria responsible for periodontitis release foul-smelling sulphur compounds, leading to persistent bad breath.
Mild Gum Recession: You might notice your teeth looking slightly longer than they used to. This is the gum tissue pulling away due to attachment loss.
Tooth Sensitivity: As gums recede, the sensitive root surfaces of your teeth can become exposed, causing discomfort with hot or cold temperatures.
Ignoring these symptoms is like ignoring a smoke detector. The problem isn't the noise; it's the potential fire it's warning you about. Understanding what happens if you have gum disease and don't treat it is crucial for your long-term health.
Risk Factors That Accelerate Gum Deterioration
While bacterial plaque is the primary cause of periodontitis, certain factors can press the accelerator on its progression, determining how quickly you might move from Stage 2 to more advanced stages. This is where a dentist considers the "grade" of your disease.
Smoking/Vaping: This is one of the most significant risk factors. Smoking impairs your body's ability to fight infection and heal, masking early symptoms like bleeding while allowing the disease to advance undetected.
Diabetes: The link between diabetes and periodontitis is a two-way street. Uncontrolled blood sugar levels make gum infections worse, and an active gum infection can make it harder to control blood sugar.
Poor Oral Hygiene: Inconsistent brushing and a lack of flossing allow bacterial biofilm to mature and become more destructive.
Genetics: Unfortunately, some people are simply more genetically susceptible to developing gum disease.
Stress: Chronic stress can weaken your immune system, making it harder for your body to combat the bacteria causing periodontitis.
Accurate Diagnosis and First-Line Treatment
If you suspect you have early periodontitis, the first step is a comprehensive professional evaluation. A standard assessment involves measuring pocket depths and taking X-rays. However, a more advanced approach can provide a far more precise diagnosis.
At The Behrens Dental Practice, we believe that to effectively treat the disease, you must first identify the exact culprit. That's why our process begins with a Micro Perio Analysis. We don't just measure pockets; we take a sample of the bacteria from your gums and perform a microbiological DNA analysis. This tells us exactly which specific bacteria are causing your infection, allowing us to create a truly personalised and targeted treatment plan.
Deep Cleanings: The Gold Standard Initial Step
For Stage 2 periodontitis, the universally accepted first line of defence is Scaling and Root Planing (SRP), often called a "deep cleaning." This isn't the same as a routine hygiene visit.
Scaling: Meticulously removes plaque, tartar (hardened plaque), and bacterial toxins from the tooth surfaces both above and below the gumline.
Root Planing: Involves carefully smoothing the root surfaces of the teeth. This helps prevent bacteria from re-attaching and allows the gums to heal and re-attach more snugly to the tooth.
SRP is designed to disrupt the bacterial ecosystem, reduce inflammation, and shrink periodontal pockets.
Advanced Non-Invasive Therapy: The Duo-Lase™ Advantage
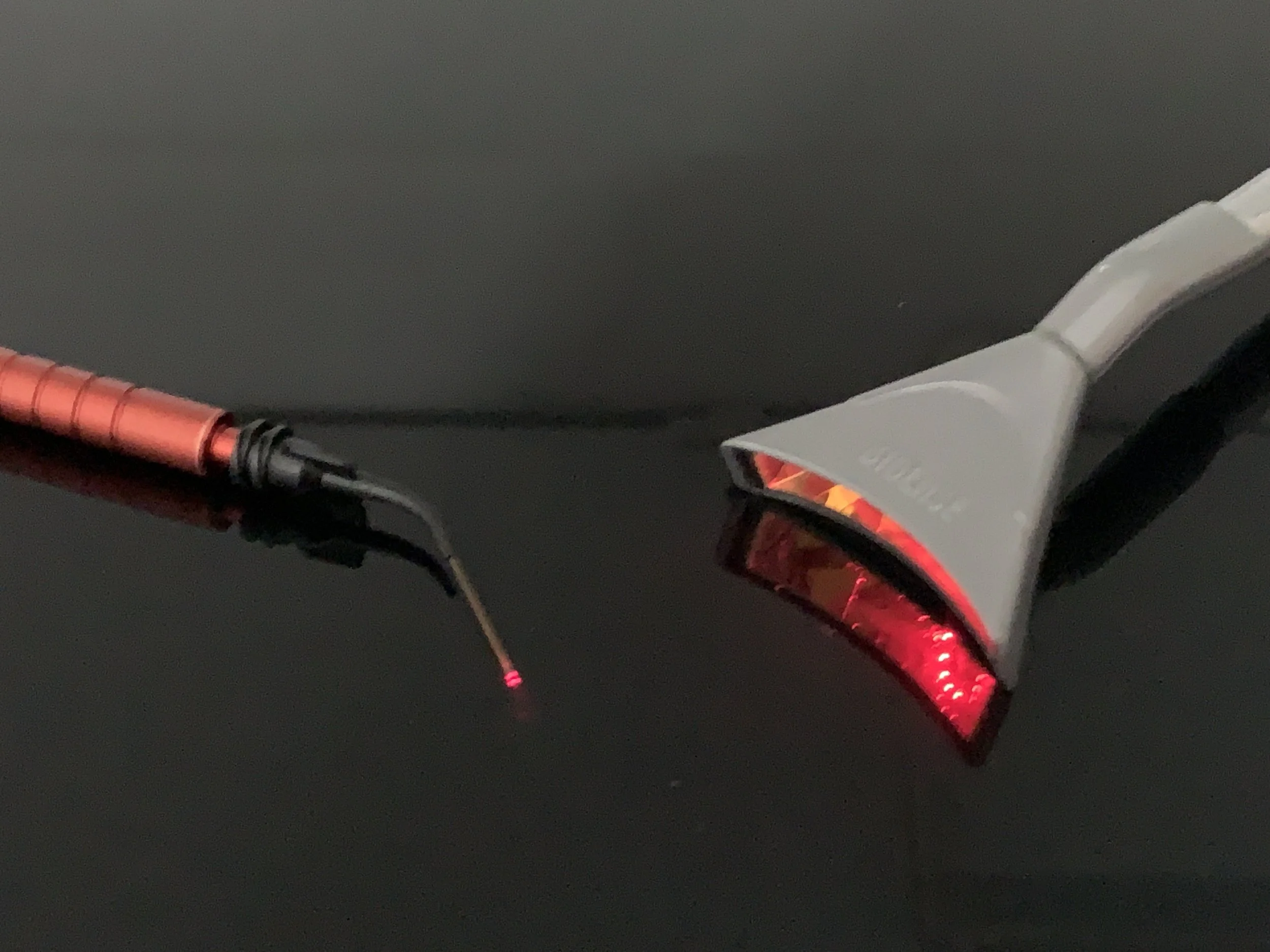
While SRP is effective, modern technology offers a way to enhance its results non-invasively. The Duo-Lase treatment is a revolutionary approach that uses two specialised lasers to combat gum disease at its source without any cutting or stitches.
Photo-Dynamic Pocket Decontamination: The first laser targets and eliminates the harmful bacteria identified in your microbiological test.
Bio-Stimulation: The second laser promotes healing, stimulates collagen production, and helps your gum tissues regenerate.
For patients in Stage 2, this Duo-Lase therapy can significantly improve outcomes, reduce discomfort, and accelerate healing, helping to halt the disease before it progresses further.
Image: https://drive.google.com/file/d/1rlsYZUgnLddnnkxtvS6GR1M-OemQ2CNc/view?usp=sharing
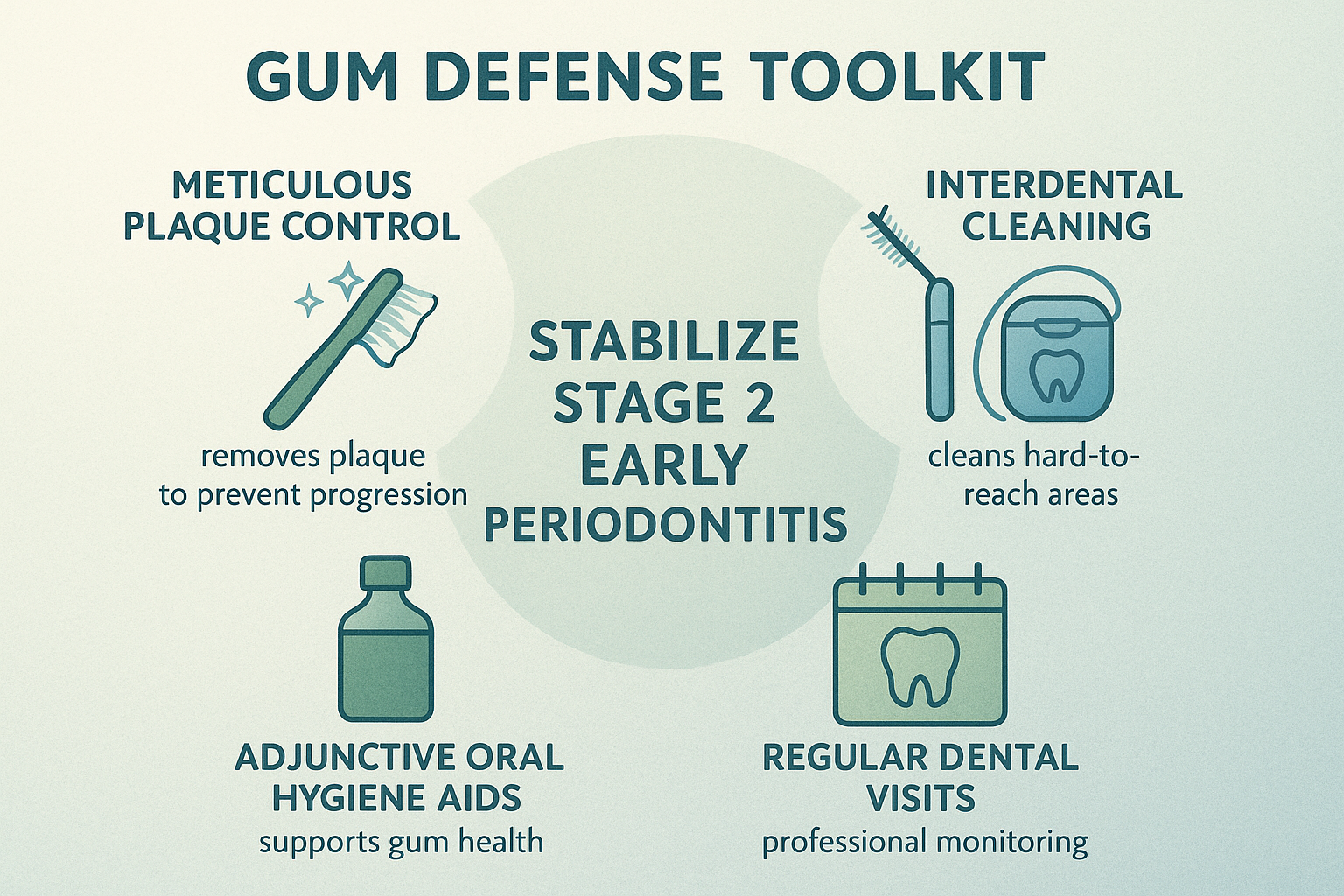
Empowering Your At-Home Defense
Professional treatment is only half the battle. What you do at home every day is what keeps periodontitis under control long-term. Stabilizing Stage 2 disease requires a meticulous commitment to oral hygiene.
Master Meticulous Plaque Control: Brush for two full minutes, twice a day, with a soft-bristled brush. Pay special attention to the gumline, where plaque accumulates most.
Clean Between Your Teeth Daily: Flossing is non-negotiable. If you struggle with traditional floss, consider interdental brushes, water flossers, or floss picks. The goal is to disrupt the bacterial colonies between your teeth that a toothbrush can't reach.
Use an Antimicrobial Mouthwash: A therapeutic mouthwash can help reduce the bacterial load in your mouth, but it is an adjunct to, not a replacement for, brushing and flossing.
Maintain Regular Professional Care: After initial treatment, you will need to see your dentist or hygienist more frequently—typically every 3-4 months—to monitor your gums and maintain your oral health.
Frequently Asked Questions
1. Can Stage 2 periodontitis be reversed?
The damage caused in Stage 2—specifically the loss of connective tissue and bone—is not fully reversible. However, with Duo-Lase, many patients have shown bone regeneration and the disease can be stabilized. With successful treatment and excellent home care, you can halt the progression, reduce pocket depths, and maintain a healthy mouth for years, preventing it from advancing to more severe stages.
2. How quickly does Stage 2 periodontitis progress?
Progression speed varies greatly depending on the risk factors involved (the "grade"). For a non-smoker with good overall health, it may progress slowly over years. For a smoker with uncontrolled diabetes, the progression can be rapid, moving to advanced stages in a much shorter timeframe.
3. Is Stage 2 periodontitis painful?
Often, it is not. This is why it's called a "silent" disease. The symptoms are typically mild, like bleeding or puffiness, which is why so many people ignore them. Pain usually doesn't become a significant factor until the disease is much more advanced.
4. Why is treating early periodontitis so important for my overall health?
The chronic inflammation associated with periodontitis doesn't just stay in your mouth. Research has linked gum disease to a host of systemic health issues, including heart disease, stroke, respiratory problems, and difficulties managing diabetes. Treating your gums is an investment in your whole-body health.
Take Control Before It Takes Hold
Stage 2 periodontitis is a critical crossroads in your oral health journey. It's the point where the path forks—one way leads towards stabilization and health, the other towards deeper pockets, significant bone loss, and ultimately, tooth loss.
The good news is that you have the power to choose your path. By recognizing the signs, understanding the risks, and seeking precise, effective treatment, you can stop this disease in its tracks. The key is to act now, while the damage is minimal and the prognosis is excellent. That little bit of pink in the sink is more than a minor inconvenience; it's a major opportunity to protect your health for a lifetime.
Understanding the process and what a treatment involves is the first step. To learn more about how a microbiological analysis and laser therapy can offer a definitive solution, a consultation can provide a clear path forward.