Understanding Gum Disease: A Beginner's Guide to What's Happening in Your Mouth.
Have you ever noticed a little pink in the sink after brushing your teeth and brushed it off as normal? Maybe you think you just brushed too hard. It’s a common thought, but it points to one of the most widespread misconceptions about oral health: that bleeding gums are no big deal.
In reality, your gums shouldn't bleed. Think of it like this: if your hands bled every time you washed them, you'd be concerned. The same principle applies to your mouth. That touch of pink is often the very first sign of gum disease, a condition that goes far beyond just your gums.
This guide is your first step to understanding what’s really going on. We’ll break down the basics in simple terms, transforming confusing dental jargon into clear, actionable knowledge.
What Is Gum Disease? A Layman’s Overview
At its core, gum disease—or periodontal disease—is a progressive inflammatory condition. It’s your body's response to a build-up of harmful bacteria in the plaque on your teeth.
Imagine your teeth are like houses. For a house to be secure, it needs a strong foundation. In your mouth, that foundation is the periodontium—a group of structures including your gums, the ligaments that hold your teeth in place, and the jawbone itself.
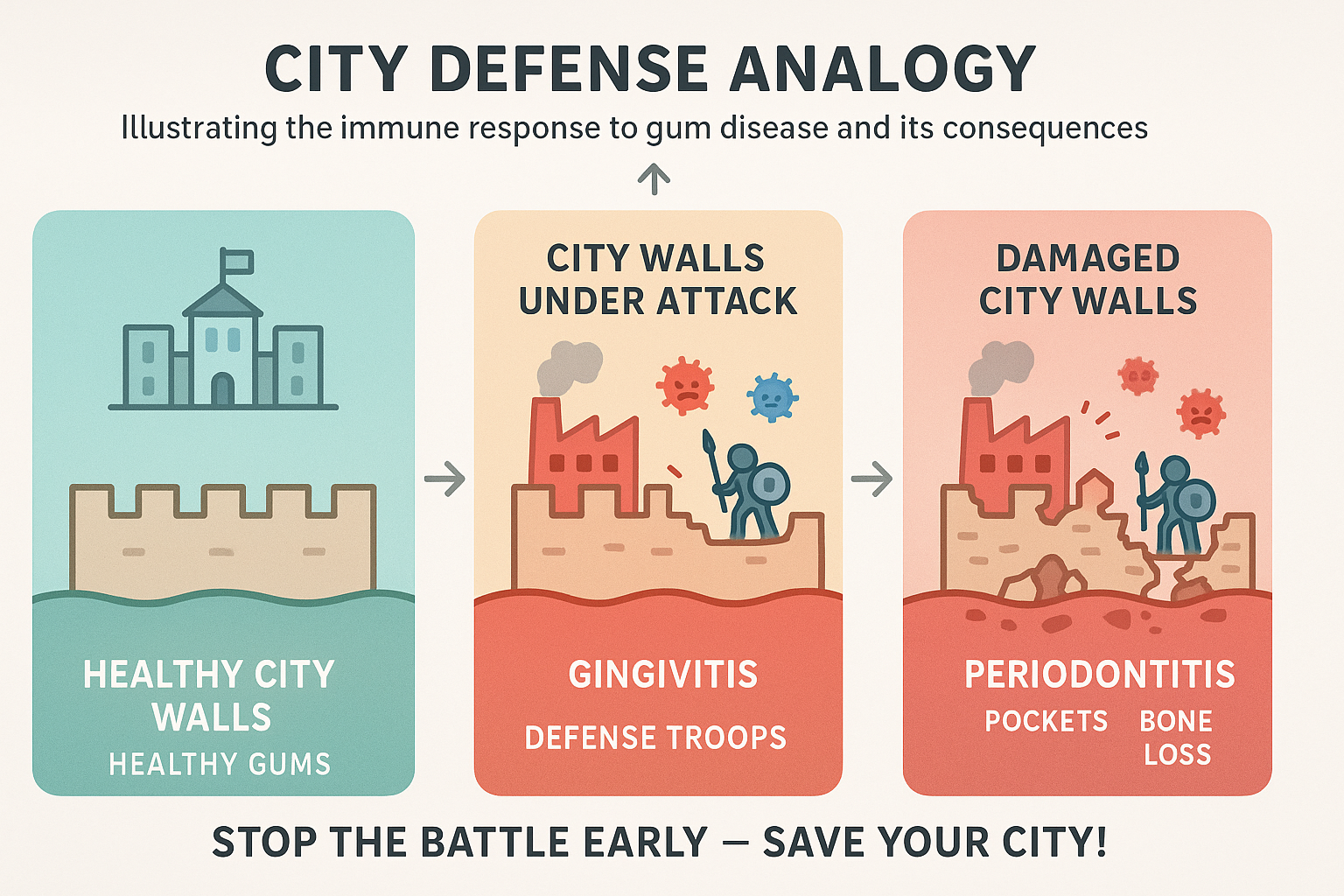
When harmful bacteria are left undisturbed, they form a sticky film called plaque. Your immune system sees this as an invasion and launches an attack. This battle causes inflammation—redness, swelling, and bleeding. Initially, this fight is confined to the gums. But if left unchecked, the chronic inflammation begins to destroy the very foundation supporting your teeth. The potential consequence of poor oral hygiene isn't just a cavity; it's the risk of losing the structures that keep your teeth stable for life.
Gingivitis vs. Periodontitis: What’s the Difference?
You’ve likely heard both of these terms, and they’re often used interchangeably. But in the world of dental health, the distinction between them is absolutely critical. It’s the difference between a small, reversible problem and a serious, irreversible one.
Gingivitis: The Early Warning Sign
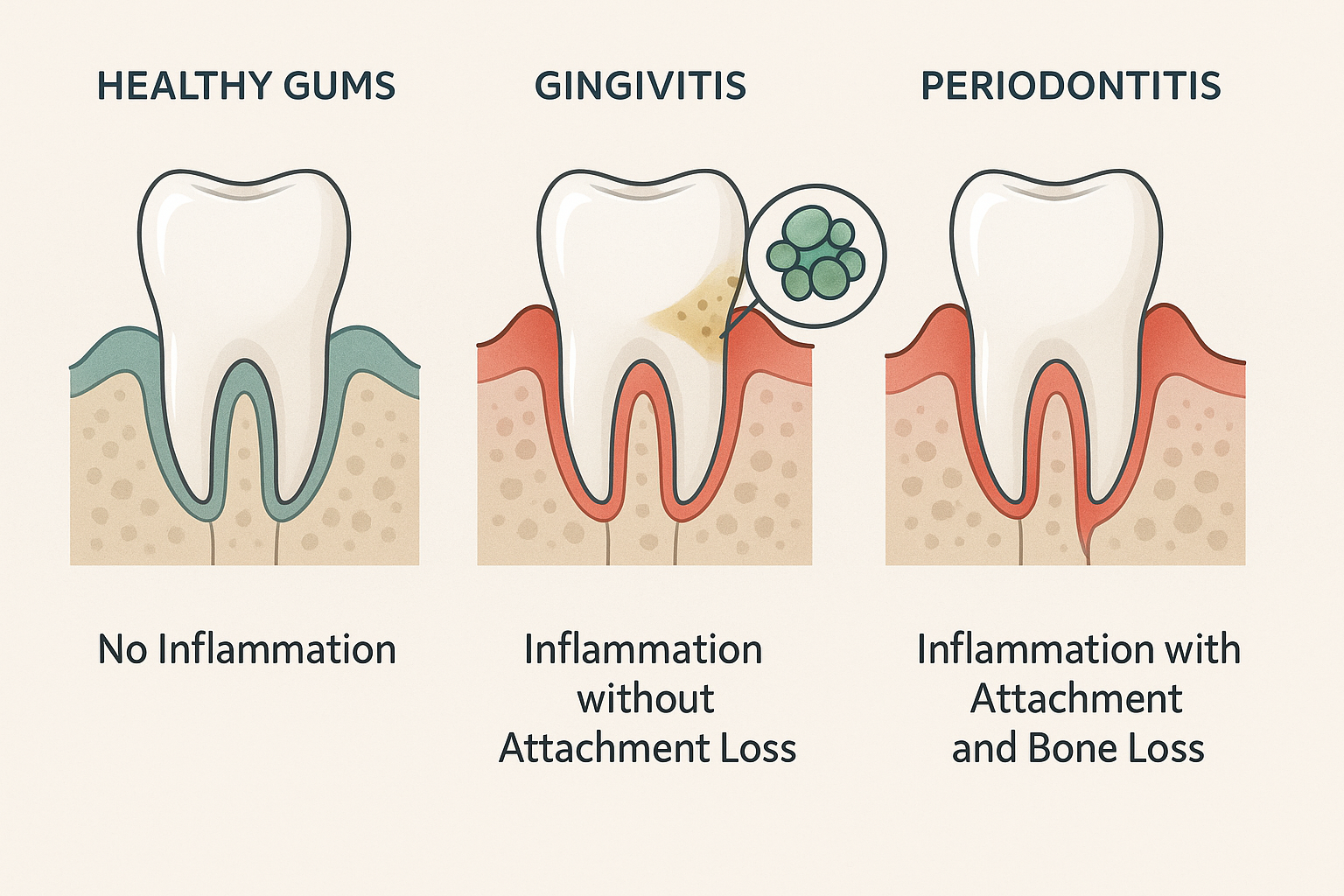
Gingivitis is the earliest and mildest form of gum disease.
What it is: Inflammation that is limited only to the gums.
The key feature: There is no "attachment loss." This means the ligaments and bone that support your teeth are still intact.
The good news: Gingivitis is completely reversible with professional cleaning and improved daily oral hygiene.
Think of gingivitis as a fire alarm. It's a loud, clear warning that there's a problem, but the house isn't on fire yet. You have time to address the issue before any permanent damage occurs.
Periodontitis: The Foundation Starts to Crumble
Periodontitis is what happens when gingivitis is left untreated. The chronic inflammation goes deeper, and the real damage begins.
What it is: The inflammation has spread beyond the gums and is now destroying the ligaments and bone that support the teeth.
The key feature: The defining characteristic of periodontitis is irreversible attachment and bone loss. Your gums start to pull away from the teeth, creating "pockets" where more bacteria can hide and cause further destruction.
This is the "aha moment" for most people. The critical difference between gingivitis and periodontitis is bone loss. While you can manage and halt the progression of periodontitis, the bone that has been lost will not grow back on its own. This is what happens if you have gum disease that progresses, and it's why early detection is so important.
Why Understanding the Stages of Gum Disease Matters
Once a dentist diagnoses periodontitis, they don’t just say, "You have gum disease." They determine its stage and grade. This isn't just medical jargon; it's a roadmap that tells you exactly where you are and what the future might hold.
Think of your tooth like a tree and your jawbone as the soil it's planted in.
Staging (Stage I-IV): This tells us how much "soil" has already eroded. It measures the severity of the damage that has already occurred, from mild (Stage I) to very severe (Stage IV).
Grading (Grade A-C): This tells us how fast the soil is eroding. It estimates the future risk of progression. Grade A is slow, B is moderate, and C is rapid progression.
Knowing your stage and grade is empowering. It helps you understand the seriousness of your condition, why a specific treatment is being recommended, and what you need to do to protect your health moving forward. It turns a vague diagnosis into a clear, personalized action plan.
The Power of a Precise Diagnosis and Advanced Treatment
Accurate staging and grading are the bedrock of effective treatment. However, at The Behrens Dental Practice, we believe in going one step further. We know that periodontal disease is caused by bacteria, but not everyone has the same type of bacteria.
That’s why our diagnostic process includes a microbiological test. This allows us to identify the specific bacterial culprits driving the disease in your mouth. Armed with this precise information—along with staging and grading—we can create a truly personalised treatment plan.
This is where innovative therapies come into play. For many patients, this tailored plan involves Duo-Lase™, a state-of-the-art dual laser treatment. This non-invasive approach is designed to:
Eliminate Harmful Bacteria: One laser specifically targets and destroys the disease-causing bacteria identified in your tests, even deep within the gum pockets where traditional tools can't reach.
Stimulate Healing: A second laser promotes tissue regeneration and collagen production, helping your body heal faster and more effectively.
By combining a uniquely precise diagnosis with advanced, minimally invasive technology, we can effectively stop periodontal disease in its tracks and create a healthy oral environment, giving you the best chance to save your natural teeth. Exploring the details of treatments like the Duo Lase can provide a clearer picture of modern periodontal care.
Frequently Asked Questions
1. What are the most common signs of gum disease?
The most common signs include red, swollen, or tender gums; gums that bleed during brushing or flossing; persistent bad breath; gums that are pulling away from the teeth (making teeth look longer); and loose or shifting teeth.
2. So, is it ever normal for gums to bleed?
No. Healthy gums do not bleed. Bleeding is a sign of inflammation and the first indicator that your gums need attention. Don't ignore it.
3. What causes gum disease besides poor hygiene?
While plaque build-up is the primary cause, other factors can increase your risk. These include smoking, genetic predisposition, hormonal changes (like during pregnancy), certain medications, and systemic diseases like diabetes.
4. Can gum disease be cured?
Gingivitis is completely curable. Periodontitis, because it involves bone loss, is not technically "curable" in the sense that the lost bone and tissue will regrow on their own. However, it can be successfully managed and its progression halted for life with proper treatment and consistent maintenance.
Your Journey to Oral Health Starts with Understanding
Taking control of your oral health begins with knowledge. You now understand that gum disease is a progressive condition, that the difference between gingivitis and periodontitis is critical, and that a precise diagnosis is the key to effective treatment.
Don’t dismiss the small signs. That pink in the sink is your body’s way of asking for help. By listening to it now, you are taking the most important step toward preserving the foundation of your smile for years to come. For more information, you can always get in touch with our team.